È un tipo di tumore molto raro (0,5-2% di tutte le neoplasie mammarie). È chiamato così perché al microscopio le cellule tumorali sono disposte in una forma che ricorda una felce. Si sviluppa di preferenza nelle donne di età >60 anni e in post-menopausa.
Il carcinoma mammario papillare può presentarsi in diversi tipi:
- Carcinoma mammario papillare invasivo
- Carcinoma mammario micropapillare invasivo
- Carcinoma papillare intracistico/incapsulato/incistato
- Carcinoma duttale papillare in situ
È spesso associato ad altri tipi di ca. mammario ed in particolare al carcinoma duttale in situ (DCIS).
EZIOLOGIA: Il carcinoma mammario papillare si verifica quando si sviluppano mutazioni nel DNA delle cellule dei dotti mammari.
DIAGNOSTICA:
- All’esame obiettivo si palpa un nodulo o ispessimento del parenchima mammario e spesso sono presenti perdite ematiche dal capezzolo e introflessione del capezzolo.
- Mammografia
- Ultrasuonografia: è la modalità di imaging più ampiamente studiata. Si evidenziano tre profili ecografici di base: (1) massa intraduttale con o senza dilatazione duttale, (2) massa intracistica e (3) modello solido con una massa intraduttale che riempie completamente il dotto. Spesso sono presenti microcalcificazioni.
- Biopsia centrale del nodulo usando un ago cavo per prelevare un campione di tessuto mammario da esaminare al microscopio
- Aspirazione con ago sottile (FNA)
Immunoistochimica – il ca. papillare è un cancro triplo negativo, (TNBC): sulle cellule tumorali non si riscontrano recettori per estrogeni (ER) nè recettori per il progesterone (PR) e non HER2. Quindi né la terapia ormonale né la terapia mirata sono efficaci. Il 10-20% di questi tumori possiedono recettori per gli androgeni (AR positivi) e da un punto di vista molecolare, questi tumori sono molto simili a quelli della prostata, e potrebbero quindi essere suscettibile agli stessi agenti terapeutici come la bicalutamide (farmaco antiandrogeno non steroideo).
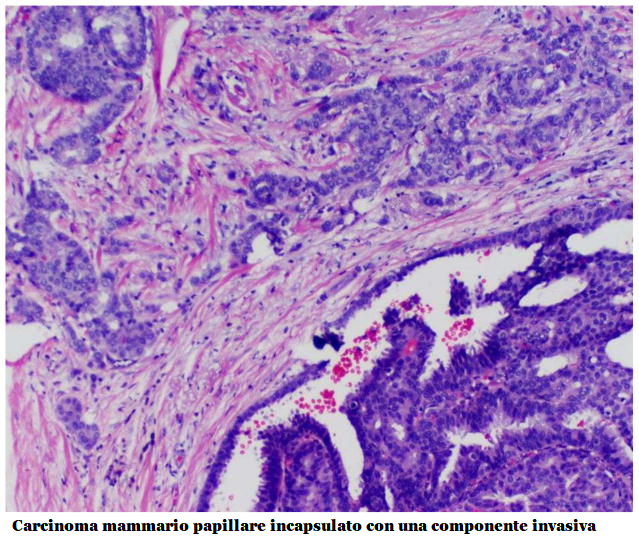
Aspetto istologico: Il carcinoma papillare solido macroscopicamente appare come noduli ben circoscritti, densamente cellulari. All’esame istologico si evidenziano proliferazioni cellulari che circondano i nuclei fibrovascolari, con o senza invasione. La mucina intracellulare ed extracellulare associata è un reperto comune. I carcinomi papillari solidi sono spesso accompagnati da aree associate di carcinoma invasivo.
TERAPIA
La chirurgia è di solito il primo e il più importante trattamento per tutti i tipi di carcinoma papillare. Viene praticata una lumpectomia oppure mastectomia se il ca. è di notevole dimensioni oppure è interessata più di un’area mammaria. A volte è necessario un ulteriore intervento chirurgico se il margine del tessuto apparentemente normale che circonda il tumore che è stato rimosso durante la prima operazione non risulta assolutamente indenne all’esame istologico.
La chemioterapia post-chirurgica migliora la sopravvivenza a 5 anni (79% vs. 69%) ed attualmente è l’unica terapia medica effettivamente disponibile.

